Would you like to see your presentation here, made available to a global audience of researchers?
Add your own presentation or have us affordably record your next conference.
Next from AMA Research Challenge 2024
poster
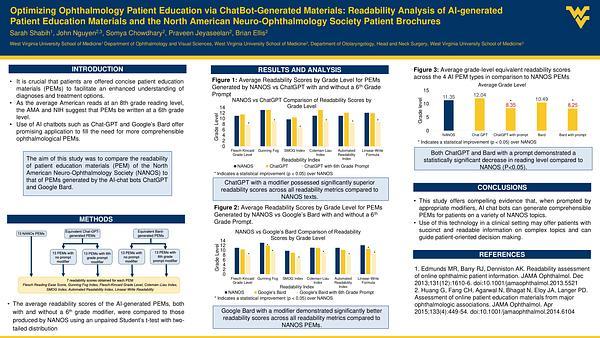
Optimizing Ophthalmology Patient Education via ChatBot-Generated Materials: Readability Analysis of AI-generated Patient Education Materials and the North American Neuro-Ophthalmology Society Patient Brochures
AMA Research Challenge 2024
SS
Sarah Shabih
07 November 2024