Would you like to see your presentation here, made available to a global audience of researchers?
Add your own presentation or have us affordably record your next conference.
Next from AMA Research Challenge 2024
poster
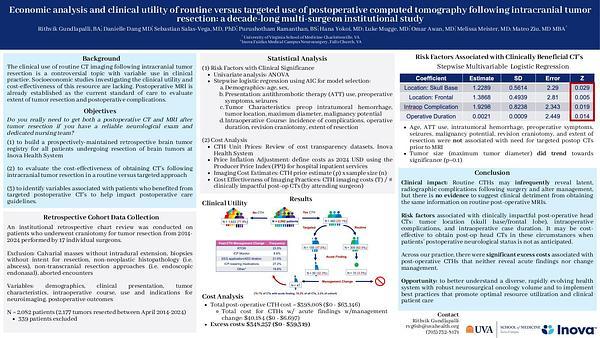
Economic Analysis and Clinical Utility of Routine Versus Targeted Use Of Postoperative Computed Tomography Following Intracranial Tumor Resection: A Decade-Long Multi-Surgeon Institutional Study
AMA Research Challenge 2024
RG
Rithvik Gundlapalli
07 November 2024